Introduction
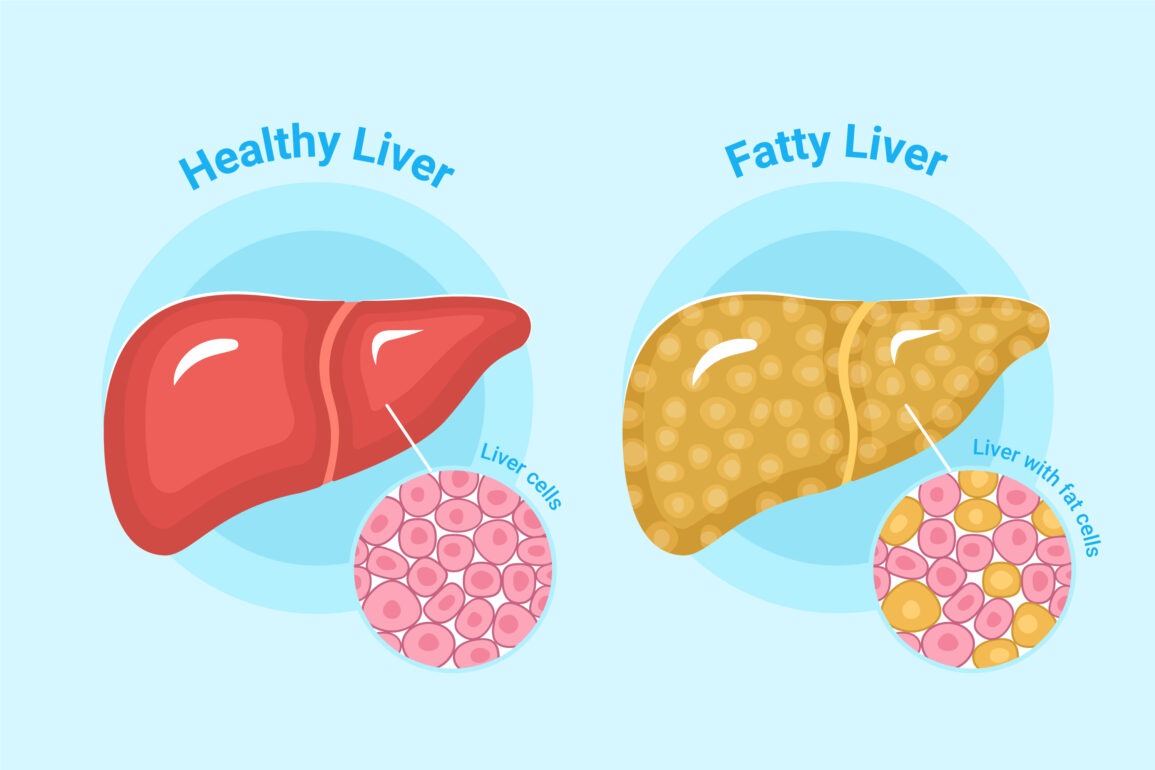
Fatty liver disease is a condition characterized by the buildup of excess fat in liver cells. While having some fat in the liver is normal, when it exceeds 5–10% of the liver’s weight, it becomes a health concern. Often described as a “silent disease,” fatty liver can progress unnoticed for years. It’s vital to understand the symptoms, causes, and preventive measures to avoid severe complications like liver failure or cirrhosis.
In this guide, we’ll delve into the symptoms, causes, risk factors, diagnosis, treatments, and prevention strategies for fatty liver disease.
Types of Fatty Liver Disease
Fatty liver disease can be categorized into two major types based on the root cause:
1. Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD occurs when fat accumulates in the liver without excessive alcohol consumption. It’s one of the most common liver conditions worldwide, often linked to metabolic disorders such as obesity, diabetes, and high cholesterol.
Characteristics of NAFLD:
- Affects individuals who consume little to no alcohol.
- Associated with poor dietary habits and sedentary lifestyles.
- Can progress to non-alcoholic steatohepatitis (NASH), leading to inflammation and scarring.
2. Alcoholic Fatty Liver Disease (AFLD)
AFLD is directly caused by excessive alcohol consumption, which disrupts the liver’s ability to process fats and toxins. Prolonged drinking causes liver cells to swell with fat, leading to inflammation and damage over time.
Characteristics of AFLD:
- Linked to heavy or binge drinking over extended periods.
- Often reversible with early alcohol abstinence.
- Can progress to alcoholic hepatitis or cirrhosis if untreated.
Symptoms of Fatty Liver Disease
One of the challenges with fatty liver disease is its often-silent nature. Symptoms may not appear in the early stages, but as the condition progresses, more noticeable signs develop. Let’s break these down:
Early Symptoms
In the initial stages, fatty liver disease is usually asymptomatic or presents mild, non-specific signs:
- Fatigue: Feeling excessively tired or weak, even after resting.
- Discomfort in the Upper Right Abdomen: A dull ache or sense of fullness caused by liver enlargement.
- Unexplained Weight Loss: Some individuals might experience an unintentional drop in body weight.
Advanced Symptoms
When fatty liver disease progresses to severe stages, such as steatohepatitis or cirrhosis, symptoms become more evident and concerning:
- Jaundice: Yellowing of the skin and eyes due to impaired liver function.
- Abdominal Swelling (Ascites): Fluid buildup in the abdominal cavity.
- Edema: Swelling in the legs and ankles caused by fluid retention.
- Mental Confusion (Hepatic Encephalopathy): Toxins in the blood lead to cognitive impairment, memory loss, or difficulty concentrating.
- Easy Bruising and Bleeding: Reduced production of clotting proteins in the liver.
Causes of Fatty Liver Disease
Fatty liver disease can result from a variety of factors, often tied to lifestyle choices or underlying health conditions:
1. Lifestyle-Related Causes
- Poor Diet: A diet high in refined carbs, saturated fats, and sugary beverages contributes to fat accumulation.
- Sedentary Lifestyle: Lack of physical activity leads to obesity and metabolic dysfunction.
2. Alcohol Consumption
Alcohol is a toxin that, when consumed excessively, overwhelms the liver’s ability to metabolize fat, resulting in fat buildup.
3. Health Conditions
- Obesity: Excess weight is a major contributor to fatty liver disease, particularly in NAFLD.
- Type 2 Diabetes: Insulin resistance interferes with how the liver processes and stores fat.
- Metabolic Syndrome: A cluster of conditions, including hypertension, high blood sugar, and abnormal cholesterol levels, increases risk.
Risk Factors
Certain risk factors make individuals more susceptible to fatty liver disease:
- Age: While fatty liver disease can occur at any age, it’s more common in adults over 40.
- Gender: Men are more likely to develop AFLD, while women face a higher risk of NAFLD.
- Family History: Genetics play a role, especially if relatives have metabolic disorders.
Diagnosis of Fatty Liver Disease
Diagnosing fatty liver disease requires a combination of medical history, physical exams, and diagnostic tests:
1. Medical History
Doctors may inquire about alcohol consumption, diet, lifestyle, and family history of liver or metabolic conditions.
2. Physical Examination
A swollen or tender liver can often be felt during an abdominal exam.
3. Blood Tests
- Elevated liver enzymes (ALT and AST) may indicate liver damage.
- Tests for triglycerides and cholesterol can identify metabolic disorders.
4. Imaging Studies
- Ultrasound: A simple and non-invasive way to detect fat in the liver.
- CT or MRI: Provides detailed images to confirm fat accumulation.
5. Liver Biopsy
A biopsy is the most definitive diagnostic method, involving the removal of a small liver sample to assess the extent of fat, inflammation, and scarring.
Treatment Options
The treatment of fatty liver disease focuses on addressing underlying causes, managing symptoms, and preventing progression.
1. Lifestyle Modifications
- Healthy Diet: Adopting a Mediterranean-style diet rich in vegetables, lean proteins, and healthy fats is highly beneficial.
- Weight Loss: Losing even 5–10% of body weight can significantly reduce liver fat.
- Exercise: Regular aerobic and resistance training improves metabolism and reduces fat.
2. Medications
Currently, no FDA-approved medications specifically target fatty liver disease, but treatments for associated conditions like diabetes and high cholesterol can help manage symptoms.
3. Surgery
For morbidly obese individuals, bariatric surgery can lead to substantial weight loss and improvement in liver health.
| Aspect | Details |
|---|---|
| Symptoms | Early Symptoms: Fatigue, abdominal discomfort. |
| Advanced Symptoms: Jaundice, swelling, mental confusion, severe abdominal pain. | |
| Causes | – Lifestyle Factors: Sedentary behavior, high-fat diets. |
| – Genetic Factors: Family history of liver conditions. | |
| – Health Conditions: Diabetes, obesity, high cholesterol, metabolic syndrome. | |
| – Alcohol Use: Prolonged excessive alcohol consumption. | |
| Risk Factors | – Obesity and overweight. |
| – Insulin resistance and type 2 diabetes. | |
| – Hypertension and high triglyceride levels. | |
| – Poor dietary habits and lack of exercise. | |
| Diagnosis Methods | – Physical Exam: Checking for liver enlargement or tenderness. |
| – Blood Tests: Elevated liver enzymes (ALT, AST). | |
| – Imaging: Ultrasound, CT, or MRI to detect fat deposits in the liver. | |
| – Liver Biopsy: Confirm inflammation, scarring, and fat content. | |
| Treatment Options | – Lifestyle Changes: Healthy eating, exercise, and weight management. |
| – Medications: For associated conditions like high cholesterol or diabetes. | |
| – Surgical Options: Bariatric surgery for obesity-related cases. | |
| – Alcohol Abstinence: Complete avoidance of alcohol for AFLD. | |
| Prevention Strategies | – Diet: Avoid saturated fats, sugar, and processed foods. |
| – Exercise: Regular physical activity to maintain a healthy weight. | |
| – Monitor Alcohol Intake: Drink in moderation or avoid alcohol entirely. | |
| – Regular Health Check-Ups: Early detection through blood tests and liver function screenings. | |
| Complications | – Liver Cirrhosis: Scarring that impairs liver function. |
| – Liver Failure: Complete loss of liver function. | |
| – Other Health Risks: Cardiovascular diseases, increased risk of liver cancer. | |
| Types of Fatty Liver | – Non-Alcoholic Fatty Liver Disease (NAFLD): Fat accumulation without significant alcohol use. |
| – Alcoholic Fatty Liver Disease (AFLD): Caused by excessive alcohol consumption. |
Prevention of Fatty Liver Disease
Preventive measures are simple yet effective in reducing your risk:
- Follow a Balanced Diet: Focus on whole foods, avoid processed snacks and sugary drinks.
- Exercise Regularly: Aim for at least 150 minutes of moderate activity per week.
- Limit Alcohol Intake: Practice moderation or complete avoidance.
- Monitor Weight: Maintain a healthy body mass index (BMI).
Complications of Fatty Liver Disease
Fatty liver disease can lead to severe health complications if untreated:
- Liver Cirrhosis: Chronic scarring disrupts normal liver function.
- Liver Failure: Complete loss of liver function, requiring a transplant.
- Increased Cancer Risk: Liver cancer is more likely in advanced cases.
Fatty Liver Disease in Different Age Groups
In Adults
Most cases occur in adults due to lifestyle factors like poor diet and lack of exercise.
In Children
Childhood obesity is on the rise, leading to an increasing number of pediatric NAFLD cases.
Advantages and Disadvantages of Fatty Liver Disease Treatments
When managing fatty liver disease, various treatment approaches come with their own set of pros and cons. Here’s a detailed look:
Advantages
- Non-Invasive Nature of Lifestyle Modifications
- Dietary changes and regular exercise are safe and non-invasive options, requiring no medical procedures.
- They address the root causes, such as obesity, insulin resistance, and poor diet.
- Improvement in Overall Health
- Weight loss, balanced nutrition, and physical activity improve not just liver health but also cardiovascular health, reduce diabetes risk, and enhance overall well-being.
- Reversibility in Early Stages
- Early intervention through lifestyle modifications or medications can reverse fatty liver disease before it progresses to severe stages like cirrhosis or liver failure.
- Cost-Effectiveness of Preventive Approaches
- Maintaining a healthy lifestyle is far less expensive than treating advanced liver conditions requiring hospitalization or surgery.
- Positive Impact on Mental Health
- Exercise and healthy living not only reduce liver fat but also boost mental health by improving mood and reducing stress.
- Availability of Support Resources
- Numerous resources, including nutritionists, fitness programs, and support groups, can aid individuals in achieving treatment goals.
- Minimized Long-Term Risks
- Early treatment reduces the risk of complications such as liver cancer or cardiovascular diseases, ensuring a longer, healthier life.
Disadvantages
- Lifestyle Modifications Require Long-Term Commitment
- Significant effort and willpower are required to sustain dietary changes and exercise routines, which can be challenging for some individuals.
- Results from lifestyle modifications may take months to become apparent, leading to frustration.
- Limited Availability of Medications
- Currently, there are no FDA-approved medications specifically for fatty liver disease, limiting treatment options.
- Drugs prescribed for associated conditions (e.g., diabetes or high cholesterol) may not directly target liver fat accumulation.
- Potential Side Effects of Medications
- Medications used to manage associated conditions, such as statins or insulin sensitizers, can have side effects like gastrointestinal discomfort, muscle pain, or liver enzyme fluctuations.
- High Costs of Advanced Treatments
- Bariatric surgery, often recommended for morbidly obese patients, can be prohibitively expensive.
- Long-term medical supervision, imaging tests, and liver biopsies may also contribute to financial burdens.
- Surgical Risks
- Bariatric surgeries or liver transplants for advanced cases come with risks like infection, complications from anesthesia, and prolonged recovery periods.
- Not all patients are suitable candidates for surgery, especially those with other underlying health conditions.
- Challenges in Diagnosing Early Stages
- Fatty liver disease is often silent, making early detection difficult. This delay can reduce the effectiveness of treatments.
- Dependency on Patient Compliance
- The success of treatments like lifestyle changes heavily depends on the individual’s commitment. A lack of motivation or understanding can hinder progress.
- Limited Success in Advanced Stages
- Once fatty liver progresses to cirrhosis or liver failure, the condition becomes largely irreversible, with treatment options focusing only on symptom management rather than a cure.
- Emotional and Psychological Strain
- Living with a chronic condition like fatty liver disease can lead to anxiety, depression, or social withdrawal, which may negatively impact treatment adherence.
Conclusion
Fatty liver disease is a silent condition that can have severe consequences if ignored. By understanding its symptoms, causes, and treatment options, you can take proactive steps to protect your liver. Early diagnosis and lifestyle changes can make all the difference in preventing complications.
FAQs
- Can fatty liver disease be reversed? Yes, early-stage fatty liver can often be reversed with lifestyle changes like a healthy diet and regular exercise.
- What foods should I avoid if I have a fatty liver? Avoid processed foods, sugary drinks, alcohol, and foods high in saturated fats.
- How is fatty liver disease different from cirrhosis? Fatty liver involves fat buildup, while cirrhosis is severe scarring of the liver.
- Is fatty liver disease common in children? Yes, especially with the rise in childhood obesity, pediatric NAFLD cases are increasing.
- Does fatty liver disease always cause symptoms? No, many people with fatty liver disease have no symptoms, especially in the early stages.